Knee joint gonarthrosis is the most common location of a degenerative-dystrophic disease, which is characterized by the gradual destruction of cartilage with consequent changes in the joint surfaces, accompanied by pain and reduced mobility.

The disease is more likely to affect women over 40 years of age, especially those with excess weight and varicose veins of the lower limbs.
The knee joint is made up of three compartments:
- medial tibiofemoral;
- lateral tibiofemoral;
- suprapatellar-femoral.
These compartments can be affected by osteoarthritis deformans (DOA) either individually or in any combination. 75% of all cases of gonarthrosis are the destruction of the medial tibiofemoral compartment (during movements, it undergoes a load that exceeds body weight by 2 to 3 times).
In young patients, only one joint is most often destroyed - the right or the left (right-sided or left-sided gonarthrosis).
Causes of knee joint DOA
Several factors may be involved in the development of degenerative cartilage changes simultaneously:
- mechanical overload of the knee joint (some specialties, sports) with microtraumatization of the cartilage;
- consequences of injuries, surgical interventions (meniscectomy);
- inflammatory diseases of the knee (arthritis);
- anatomical inconsistencies of joint surfaces (dysplasia);
- violation of statics (flat feet, curvature of the spine);
- chronic hemarthrosis (accumulation of blood in the synovial cavity);
- metabolic pathology (gout, hemochromatosis, chondrocalcinosis);
- excess body weight;
- violations of the blood supply to the bone;
- osteodystrophy (Paget's disease);
- neurological diseases, loss of sensation in the limbs;
- endocrine disorders (acromegaly, diabetes mellitus, amenorrhea, hyperparathyroidism);
- genetic predisposition (generalized forms of osteoarthritis);
- violation of collagen type II synthesis.
But in 40% of cases, it is impossible to establish the root cause of the disease (primary arthrosis).
Pathogenesis of gonarthrosis
initial state
At the initial stage of the disease, the processes of cartilage metabolism are disturbed. The synthesis and quality of the main structural unit of cartilage tissue, the proteoglycans, responsible for the stability of the collagen network structure, are reduced.
As a result, chondroitin sulfate, keratin and hyaluronic acid are washed out of the mesh and structurally defective proteoglycans can no longer retain water. It is absorbed by collagen, whose swollen fibers lead to a decrease in cartilage's resistance to stress.
In the synovial cavity, pro-inflammatory substances accumulate, under the influence of which the cartilage is destroyed even more quickly. Joint capsule fibrosis develops. The change in the composition of the synovial fluid makes it difficult for the cartilage to deliver nutrients and impairs the sliding of joint surfaces during movement.
Progression of pathology
In the future, the cartilage gradually becomes thinner, it becomes rough, cracks form throughout its thickness. The epiphyses of bones undergo an increased load, which causes the development of osteosclerosis and compensatory proliferation of bone tissues (osteophytes).
This body reaction aims to increase the area of the joint surfaces and redistribute the load. But the presence of osteophytes increases discomfort, deformity and further limits limb mobility.
Microfractures are formed in the thickness of the bone, which injure the vessels and lead to intraosseous hypertension. In the last stage of osteoarthritis, joint surfaces are completely exposed, deformed, limb movements are severely limited.
Symptoms of gonarthrosis of the knee joint
Osteoarthritis of the knee joint is characterized by a chronic and slowly progressive course (months, years). The clinic grows gradually, without pronounced exacerbations. The patient cannot remember exactly when the first symptoms appeared.
Clinical manifestations of gonarthrosis:
- pain. At first, diffuse, short (with prolonged standing, climbing stairs), and as osteoarthritis progresses, the pain becomes local (front and inner surface of the knee), its intensity increases;
- local tenderness to palpation. Mainly on the inside of the knee along the edge of the joint space;
- crushing. In stage I it may be inaudible, in stage II-III it accompanies all movements;
- swelling, knee deformation. As a result of weakening of the lateral ligaments, a person develops an O-shaped configuration of the limbs (it is clearly visible even in the photo);
- mobility restriction. At first, there are difficulties in bending the knee, later - with extension.
Causes of pain in DOA:
- mechanical friction of damaged joint surfaces;
- increased intraosseous pressure, venous congestion;
- synovitis adhesion;
- changes in periarticular tissues (stretching of the capsule, ligaments, tendons);
- periosteal thickening;
- dystrophy phenomena in adjacent muscles;
- fibromyalgia;
- compression of nerve endings.
Unlike coxarthrosis, knee AOD may show spontaneous regression of symptoms.
Clinical manifestations of gonarthrosis depending on the stage:
| Features | I stage | II stage | III stage |
|---|---|---|---|
| Pain | Short, most often occurs when the knee is extended (standing for a long time, walking up stairs) | Moderate, disappears after a night's rest | Pronounced, disturbing even at night |
| mobility restriction | not visible | There is an extension restriction, mild lameness | Persistent flexo-extensor contractures, claudication |
| grinding | No | Sensitive to palpation during movement | remote shredding |
| Deformation | Absence of | Slight limb axis deviation anteriorly, muscle wasting | Valgus or varus deformity. Joint is unstable, atrophy of thigh muscles |
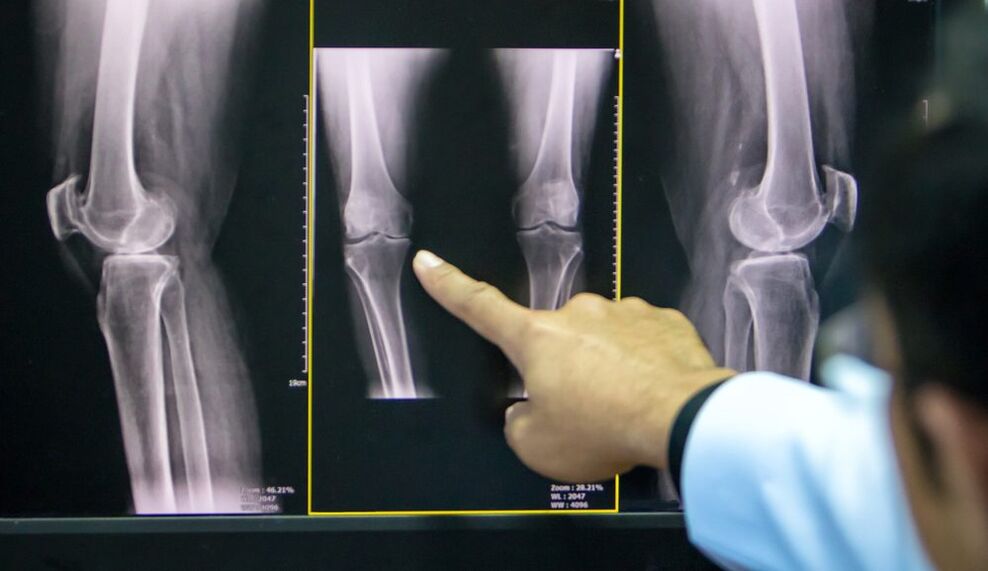
| x-ray image | Slight joint space narrowing, early signs of subchondral osteosclerosis | Joint space is reduced by 50% or more, osteophytes appear | Nearly complete absence of joint space, significant deformation and sclerosis of joint surfaces, areas of subchondral bone necrosis, osteoporosis |
A frequent complication of osteoarthritis of the knee joint is secondary reactive synovitis, characterized by the following symptoms:
- growing pain;
- swelling;
- effusion in the synovial cavity;
- increase in skin temperature.
Less frequent and more dangerous complications include: joint blockage, osteonecrosis of the femoral condyle, patellar subluxation, spontaneous hemarthrosis.
Diagnosis of AOD of the knee joint
The diagnosis of gonarthrosis is based on the patient's characteristic complaints, on the changes detected during the examination and on the results of complementary exams.
To confirm osteoarthritis, it is prescribed:
- radiography of the knee joint in two views (anteroposterior and lateral): the most accessible way to confirm the diagnosis in the advanced stage of the pathology;
- Ultrasonography: determination of the presence of effusion in the joint, measurement of cartilage thickness;
- synovial fluid analysis;
- diagnostic arthroscopy (visual assessment of cartilage) with biopsy;
- Computed tomography and magnetic resonance imaging (CT, MRI): the best method for diagnosing AOD in the early stages.
If the doctor has doubts about the diagnosis, it may be prescribed:
- scintigraphy: scanning the joint after the introduction of a radioactive isotope;
- thermography: study of the intensity of infrared radiation (its strength is directly proportional to the strength of inflammation).
Treatment of gonarthrosis of the knee joint
The osteoarthritis treatment regimen combines several approaches: non-drug methods, pharmacotherapy, and surgical correction. The proportion of each method is determined individually for each patient.
non-drug treatment
In the latest ESCEO (European Society for the Clinical Aspects of Osteoporosis and Osteoarthritis) guidelines on how to treat osteoarthritis of the knee, experts place special emphasis on patient education and lifestyle modification.

The patient needs:
- explain what the essence of the disease is, configured for long-term treatment;
- teach how to use assistive devices (canes, orthoses);
- prescribe a diet (for patients with a body mass index greater than 30);
- give a set of exercises to strengthen the thigh muscles and unload the knee joint;
- explain the importance of increasing physical activity.
In the early stages of knee arthrosis, physiotherapy treatment methods give good results:
- massage;
- magnetotherapy;
- UHF therapy;
- electrophoresis;
- hydrogen sulphide baths;
- paraffin applications;
- acupuncture.
Pharmacotherapy of gonarthrosis
The use of drugs in DOA is aimed at relieving pain, reducing inflammation, and decreasing the rate of cartilage destruction.
Symptomatic treatment:
- analgesics;
- non-steroidal anti-inflammatory substances (NSAIDs) from the group of COX-2 inhibitors in the form of tablets or suppositories;
- non-narcotic analgesics (with resistant pain syndrome).
Structure modifying drugs (chondroprotectors):
- Chondroitin sulfate;
- Glucosamine sulfate.
These drugs can be taken in the form of capsules in courses several times a year, injected intramuscularly or directly into the synovial cavity.
Local therapy includes close and intra-articular injections of glucocorticosteroids, hyaluronic acid preparations.
In stages I-II of DOA, an important place in complex therapy is the use of NSAID-based anti-inflammatory ointments, gels and creams. They help reduce the patient's need to take NSAIDs by mouth, thus reducing the risk of damage to the digestive tract.
Folk remedies
The use of tinctures, decoctions, extracts, local applications of medicinal plants should be considered as auxiliary methods for the treatment of DOA, folk remedies cannot replace the therapy prescribed by the doctor.
Plants used in osteoarthritis: dandelion, ginger, Jerusalem artichoke, burdock, garlic, hawthorn.
Surgery
Surgical intervention may be necessary in all stages of gonarthrosis with insufficient effect of medical measures. The most common are endoscopic procedures, in the most severe cases, endoprosthesis replacement is indicated.

Types of endoscopic interventions:
- joint revision and rehabilitation: extraction of inflammatory contents from the synovial cavity, cartilage fragments;
- plasma or laser ablation: removal of mechanical obstructions in the synovial cavity;
- chondroplasty.
Corrective periarticular osteotomy is indicated for patients with initial manifestations of axial limb deformity (no more than 15-20%).
The purpose of the operation is to restore the joint to normal configuration, evenly distribute the load over the joint surface, and remove damaged areas. This procedure allows you to delay the arthroplasty.
Indications for replacing the affected area (or the entire joint) with an artificial one:
- DOA grade II-III;
- severe axial limb deformity;
- aseptic necrosis of the subchondral bone layer;
- persistent pain syndrome.
Contraindications for knee arthroplasty:
- total damage to the joint;
- unstable ligament apparatus;
- DOA as a consequence of inflammatory arthritis;
- persistent flexion contracture, severe muscle weakness.
In this case, the patient undergoes arthrodesis - a comparison of the knee joint in a physiological position with the removal of the joint surfaces. This relieves pain but shortens the leg, causing secondary injuries to the contralateral knee, hip, and spine.
Prevention
Prevention of premature cartilage degeneration should begin in childhood.
Precautionary measures:
- scoliosis prevention;
- correction of flat feet (shoes with arch support);
- regular physical education (limit heavy sports);
- exclusion of fixed postures during work.

























